Bone Fracture Repair Anatomy: 3 Ways to Categorize Bone
In order to understand what role bone graft products carry in the process of bone fracture repair, it is important to understand the architecture of bone and the different categories of bone involved in the healing process. Like most complex subjects, there are many ways to characterize bone. This blog describes the three main methods of categorizing bone.
- Macroscopic Appearance: Cancellous Bone vs. Cortical Bone
- Degree of Maturity: Woven vs. Lamellar Bone
- Embryological Development: Membranous vs. Endochondral Bone
Macroscopic Appearance: Cancellous Bone vs. Cortical Bone
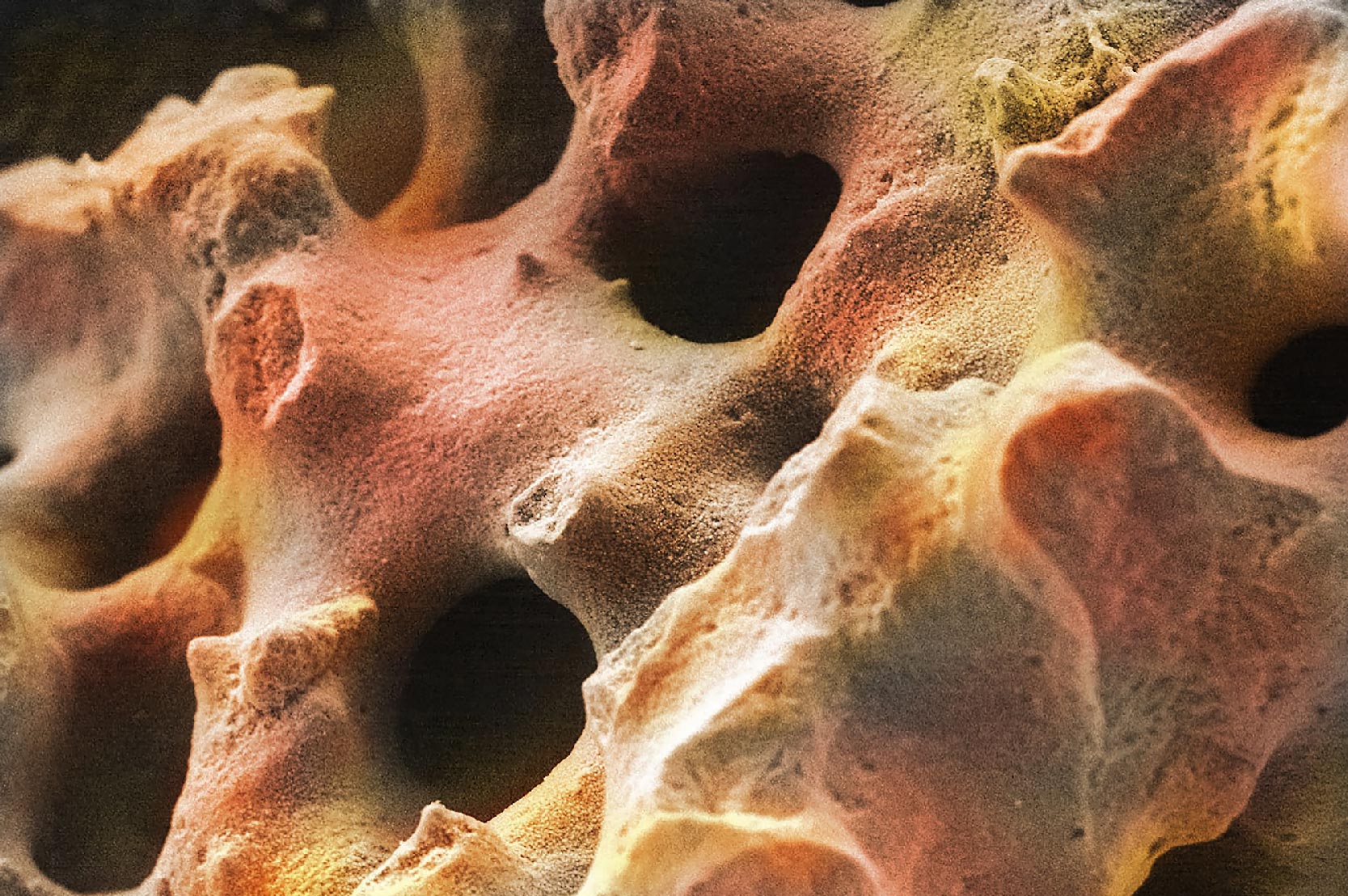
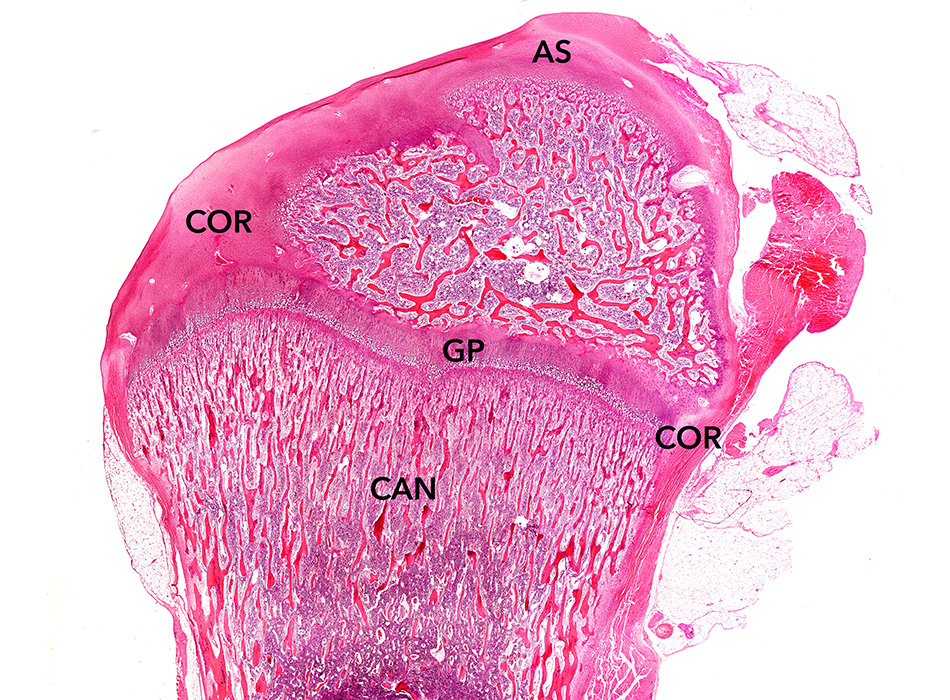
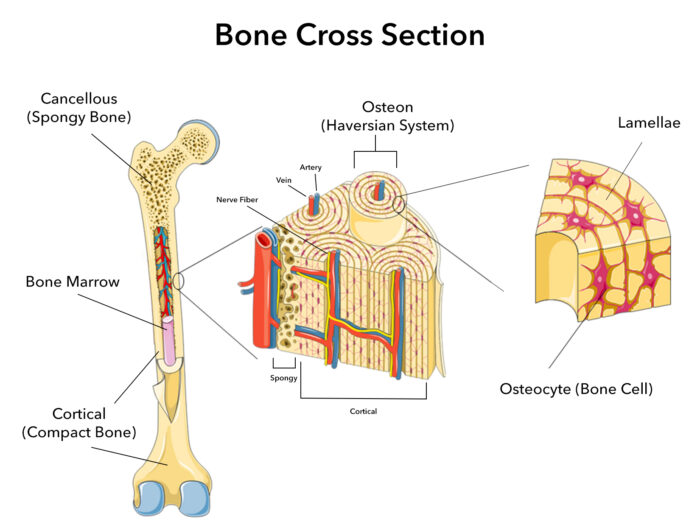
On the macroscopic level, bone can be classified as either cancellous bone or cortical bone. Synonyms for cancellous bone are trabecular or spongy bone. Cortical bone may be referred to as dense or compact bone. When looking at bones with an unaided eye, it is easy to see distinct differences in the porosity or density. Cancellous bone tissue is typically found on the interior of the bone whereas cortical bone is found on the exterior (Figure 1). With a severe bone fracture, often both cortical and cancellous bone are broken.
Cancellous bone porosity typically ranges from 75-95% with an average pore size of 200-600μm in diameter. This gives it a honeycombed, spongy appearance and light weight. It is found in the inner chamber of most bones, typically at the ends, near joints. This type of bone is made out of trabeculae, which are curved beams or arches arranged specifically to evenly distribute biomechanical loads onto the articular surfaces of joints.
Cancellous bone’s low density causes it to be more fragile than cortical bone, but it is also more flexible. In engineering terms, it has a lower modulus of elasticity. This cushioning effect prevents or delays arthritis of the more fragile and non-regenerative tissues, specifically cartilage or spinal discs. Cancellous bone’s high level of porosity also serves as a reservoir for bone marrow, which is vital for the regeneration of a variety of tissues. Lastly, cancellous bone serves as a source for storing calcium and phosphorus for use throughout the body.
In contrast to cancellous bone, cortical bone is very dense being only 5-10% porous. Therefore, it is heavier in weight. The pores are very small, typically ranging from 10-100μm in diameter. In fact, the pores sizes of the channels that feed the osteocytes, called canaliculi, are less than 500 nm (0.5μm). For the most part, the pores of cortical bone are not visible without magnification. These pores are just large enough in diameter to allow blood and lymphatic vessels, as well as nerves, to snake throughout cortical bone to support all the osteocytes and other cells found in bone. Due to its high density, cortical bone serves as a hard protective layer around the internal bone marrow cavity and carries most of the biomechanical loads applied to our bones.
Degree of Maturity: Woven vs. Lamellar Bone
After a major bone fracture, the body races to repair the fracture to avoid a permanent non-union. If the body is able to repair the bone fracture and create a union, mature bone formation goes through two stages.
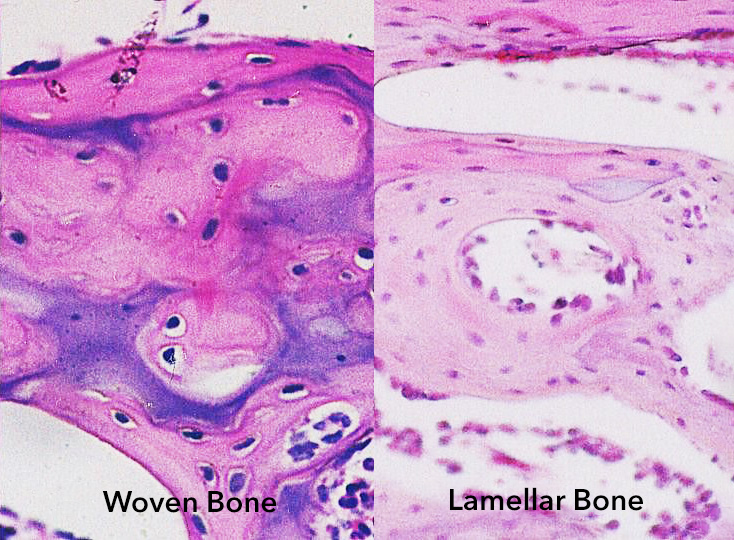
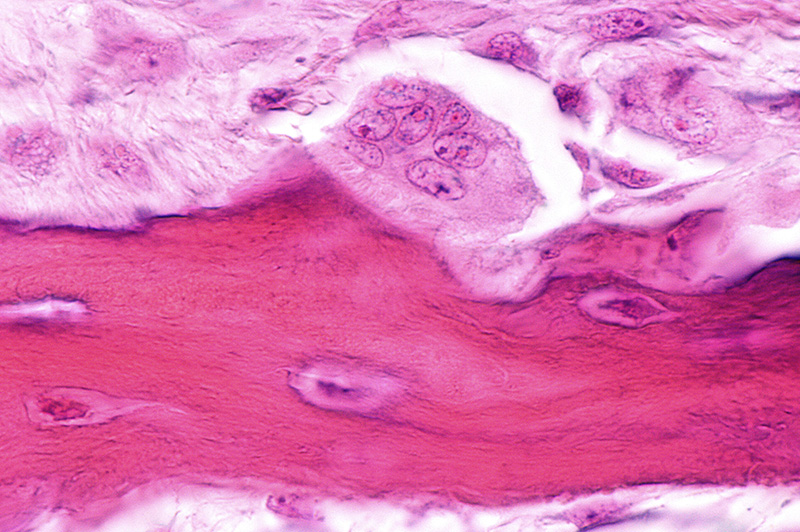
After disruption of a bone, the bone fracture repair process usually results in formation of woven bone at the site of a healing bone fracture. Woven bone is immature bone with a haphazard or random organization of collagen fibers, which means it is a mechanically weak pattern. It is not optimized for strength. Instead, it represents the body’s quick but temporary solution to return to function. Over time, bone cells remodel the woven bone into a more organized form – lamellar bone. Lamellar bone contains osteons, also known as Haversian systems (Figure 1). Virtually, all bone in a healthy adult is lamellar.
With lamellar bone, the collagen fibers are aligned into parallel sheets, called lamellae. The lamellar pattern provides extra strength similar to the way laminated plywood functions. Moreover, the collagen becomes more mineralized over time. It converts from “osteoid,” to mature, lamellar bone. Osteoid means that the early bone looks superficially like bone but is not fully mineralized. Consequently, after remodeling from woven bone to lamellar bone, the proportion of bone relative to surrounding tissue decreases as anticipated by Wolff’s Law (Wolff’s Law describes how mechanical strains on the cell membrane activate bone’s ability to form more bone in response to stress). This is because lamellar bone is mechanically a much stronger form (Figure 2).
Embryological Development: Membranous vs. Endochondral
In utero, our bones are formed by two very different embryological processes: either as endochondral bone or as membranous bone. Endochondral bone forms through a cartilaginous phase. That is, cartilage is formed first. This early tissue then gets remodeled during fetal development to a fully formed bone. The vast majority of human bones form though this endochondral process. Examples of endochondral bone are the long bones, such as femur or humerus, but also smaller bones, such as the digits of the hand.
In contrast, membranous bone forms when stem cells and osteoblasts directly form lamellar bone. The best examples of membranous bone are the cranium or sternum.
The reason why it is important to understand the difference between membranous and endochondral bone formation is that bone fracture repair can progress through either of these two mechanisms at any stage of life. Understanding how bone forms provides insight into the mechanisms of action for different types of bone grafts and how best to treat patients.
Image sources:
- File is licensed under the CC Attribution-Share Alike 4.0 International license. Brightness and text adjustments were made. Original image available at: https://josr-online.biomedcentral.com
As a recognized leader in advanced bone graft technologies, Biogennix is committed to bringing high-quality educational content to our field. This blog will cover technical topics ranging from basic bone graft science to advanced osteobiologic principles. We’ll also discuss market trends and industry challenges. We thank you for reading and invite you to learn more about us here.