Bone Remodeling Process: Bone Resorption
Earlier blog posts have explained the processes of bone modeling and bone remodeling. Whether bone is modeling or remodeling depends on the balance of bone formation and bone resorption. This blog will describe these cellular processes in detail and provide background for a more detailed understanding of how bone formation and bone resorption impact bone graft materials.
Bone Remodeling vs. Bone Modeling
When using bone graft materials, it is important to understand how bone remodeling and bone modeling work, because these two processes impact how the body responds to bone graft materials. An ideal bone graft material’s primary function is to regenerate normal bone and to respond exactly like normal bone would respond.
To proceed, we must first learn the difference between bone remodeling and bone modeling.
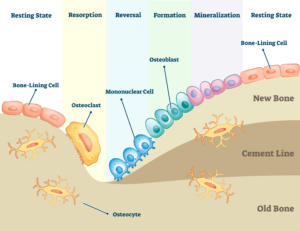
- Bone Remodeling: Bone remodeling is the normal repair process that occurs throughout life to renew tiny defects in the bone resulting from normal wear and tear of our skeleton. Remodeling also maintains vascular homeostasis of certain elements that are important throughout the body. For example, calcium and phosphorus are essential elements that circulate in the blood but are stored in bone. Bone remodeling occurs when there is a balance between new bone formation by osteoblasts and old bone resorption by osteoclasts (Figure 1). When a balance exists, there is no net change in bone mass. There are, however, instances when either one of these processes overtakes the other. This is referred to as bone modeling.
- Bone Modeling: Bone modeling occurs when the bone formation and bone resorption phases are out of balance. An example of this is the decrease in bone mass due to excessive proliferation of osteoclasts, which can cause medical conditions such as osteoporosis. Conversely, increases in bone mass can occur in response to increased mechanical loads on the skeleton which stimulates osteoblasts and increases bone formation. This can occur through an increase in exercise, such as with weightlifting or high impact training.
Physiology of Bone Remodeling
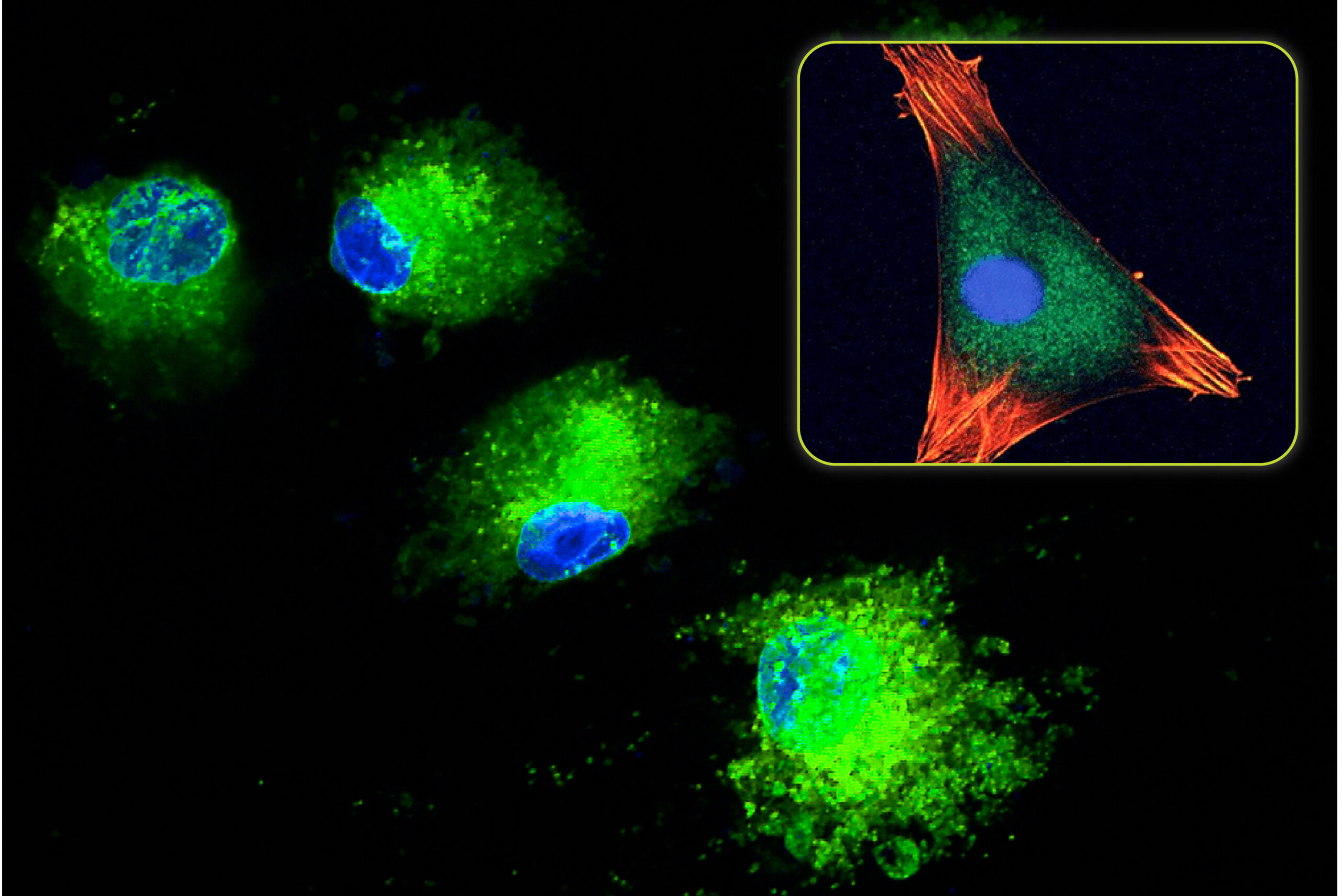
Bone remodeling requires all three types of bone cells – osteocytes, osteoblasts, and osteoclasts – to work together. Like most cells, bone cells are stimulated or suppressed by a complex set of signaling factors, i.e., systemically or locally secreted proteins or peptides. There are five stages that bone goes through when it remodels. These stages are illustrated in Figure 1.
As covered in a previous blog about Bone Physiology – Bone Matrix, bone is mostly composed of osteocytes entrapped in a boney matrix. These osteocytes are essentially dormant or hibernating. Periodically, these “resting” osteocytes are stimulated to move into a “resorption” phase. The resorption phase can be initiated when the resting osteocytes sense microstrains. Microstrains are tiny mechanical loads that cause tugging on their cell membranes, often due to increased biomechanical loads or microfractures due to everyday wear and tear. Resorption may also be initiated by the endocrine system which releases hormones into the blood. These hormones signal bone either to release calcium or to store calcium, in order to maintain homeostasis of the blood. Interestingly, certain nanostructured surfaces can also cause bone cells to “think” they are being loaded due to stretching of the cell membrane once it contacts the nano-sized structures. This is a beneficial property of advanced bone graft materials that is covered in a previous blog on the Effect of Surface Composition on Bone Formation.
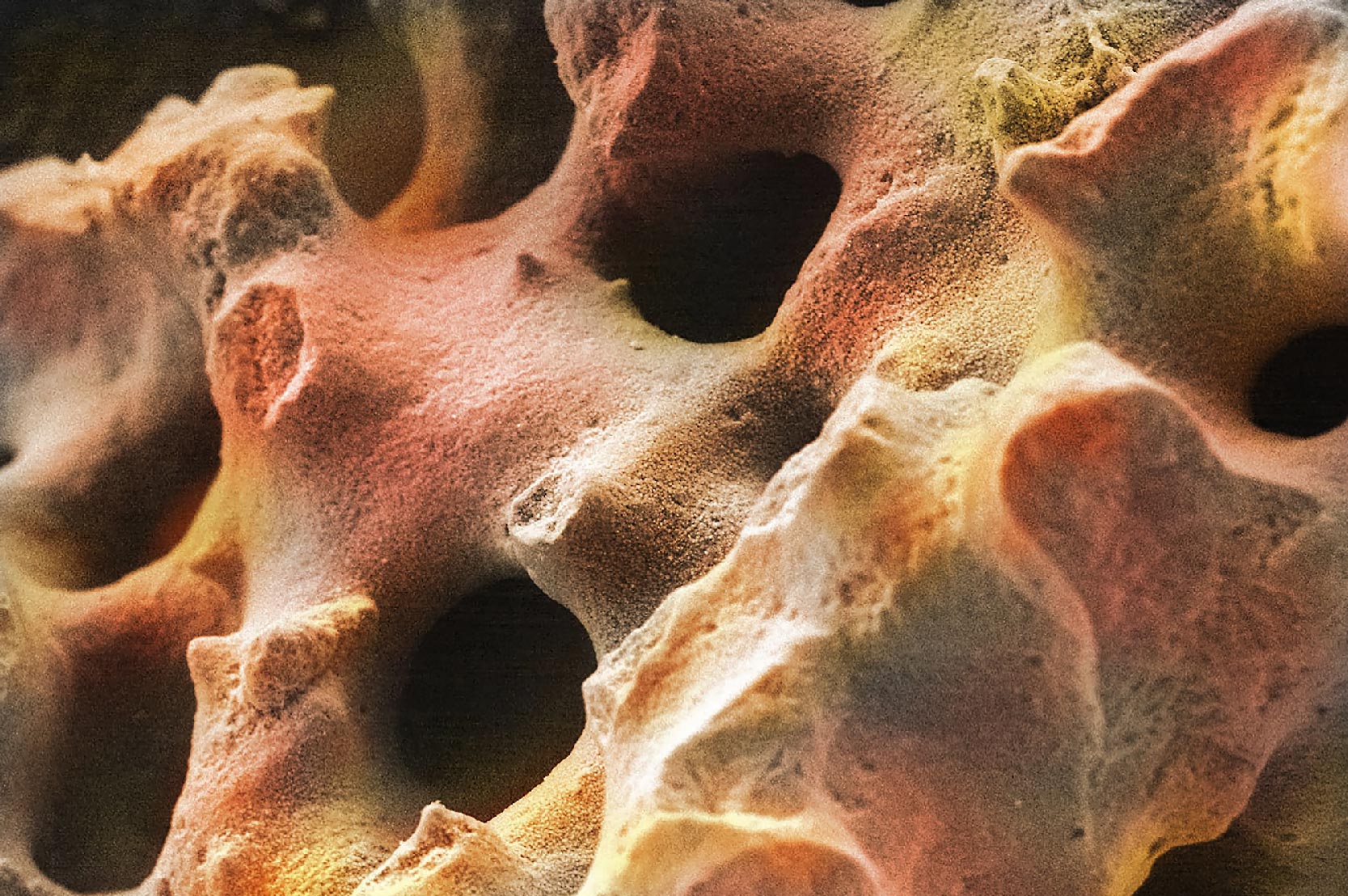
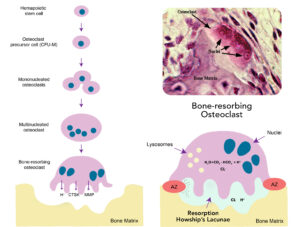
To initiate the resorption phase, multinucleated osteoclasts are formed by cell–cell fusion of mononuclear preosteoclasts in the blood. Although most osteoclasts contain only 2 to 12 nuclei (chromosome-containing organelles), some may have as many as 200 nuclei. The osteoclast’s job is to then secrete a high concentration of hydrochloric acid and enzymes from their cell membrane to dissolve a small area of the old bone forming a pit, called Howship’s lacunae (Figure 2). The hydrochloric acid dissolves the mineral content of bone to create the pit. This excretion of hydrochloric acid from the cytoplasm is very similar to the way cells of the stomach secrete large volumes of very powerful hydrochloric acid for digestion of a variety of foods.
However in bone, to prevent the acid from escaping, tiny attachments between the osteoclast cell membrane and the bone seal off the acid and enzymes to increase their concentration. Due to this cellular process, resorption ends up being very controlled.
Once a resorption pit has been created, new bone needs to form in order to maintain bone mass. To initiate the growth of new bone, osteoclasts secrete growth factors that instruct circulating mesenchymal stem cells in the bone marrow to form into osteoblasts. These are cells that build new bone. The osteoblasts migrate to the resorption site so they can proliferate and begin laying down new bone. This is called the “reversal” phase (Figure 1). Osteoblasts can also migrate from the lining of bone, such as the periosteum, to participate in the new bone formation process. It is important to remember that all cells require a network of capillaries to bring vital nutrients, eliminate waste products, and to provide essential cells for supporting tissue growth.
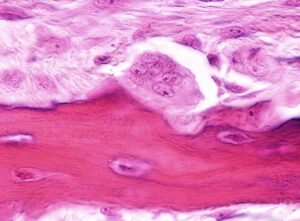
After the osteoblasts form new bone, they either die, become osteoblastic lining cells in the periosteum, or become mature osteocytes (“mineralization” phase, Figure 1). These osteocytes can “awaken” at a later date to restart these remodeling phases. As a result, the five phases are a cycle, not a linear process. In humans, the cycle is variable in time but takes approximately 120-200 days to complete.
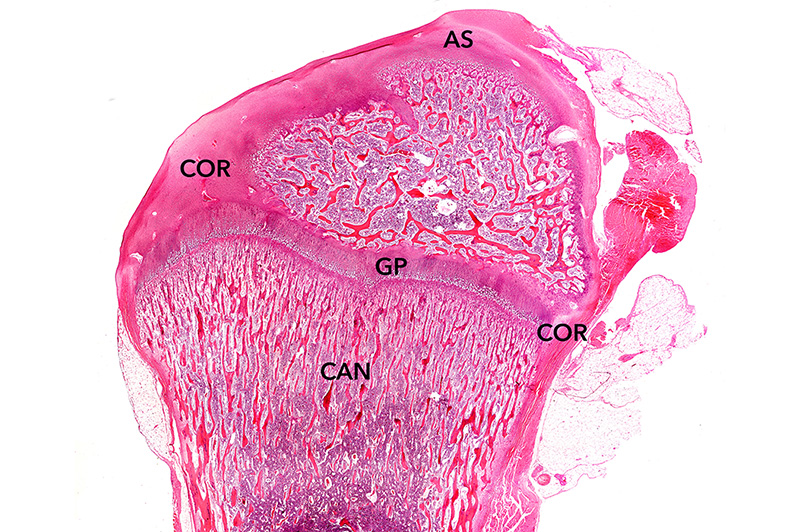
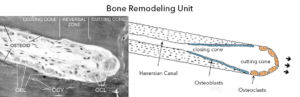
Bone remodeling literally cuts “tunnels” into the bone. However unlike a mechanical tunneling machine, it simultaneously fills in the tunnel with a new rejuvenated bone matrix. When bone cells work together to remodel bone, they are referred to as “cutting cones” when looked at under the microscope by anatomists. As shown in Figure 3, they look like actual cones that are cutting into old bone. It is estimated that there are more than one million of these bone metabolic units throughout the human body at any point in time.
Why Resorption of Bone is Important
You might ask why the body spends so much time and energy remodeling our skeletal system. The answer is that vertebrates, including humans, are in a constant state of motion. Consequently, our bones are undergoing microscopic fatigue fractures that can, just like a bridge that is not well maintained, fail spontaneously, i.e., stress fracture. They can also fail due to a high energy impact, as in the case of a traumatic injury. Like a bridge, the human body is overbuilt to easily support normal day to day loading, but there is a limit to how much extra weight we can safely carry around. Evolution has determined that remodeling is a better tradeoff than building an indestructible skeleton. On average, the human body recycles its bones through this process of remodeling at least once every 10 years, and much more rapidly during the teenage years.
The other major reason for having a bone remodeling process is that the body is able to store and retrieve key elements required for other bodily processes. For example, calcium (Ca), a key element found in the mineral component of bone, also plays an important role in other body processes like blood clotting, helping muscles to contract, and regulating normal heart rhythms and nerve functions. Similarly, phosphorus (P), which is also stored in bone and is an essential element for bone structure, is crucial for the membrane function of nerves and muscle, as well as for metabolism of key macromolecules like ATP. When the body needs these elements, resorption may be initiated to release them from bone and into our bloodstream. To do so, certain hormones such as parathyroid hormone (PTH), can increase resorption, causing increases in blood calcium and phosphorus. Conversely, other hormones such as calcitonin have an opposite effect and decrease resorption, thereby preserving these elements in bones.
What Factors Can Impact Bone Resorption?
Disease can distort the balance of bone formation and resorption. For example, osteoporosis is caused by excessive osteoclastic activity due to normal aging, decreased physical actively, genetics, or hormonal changes. Conversely, exercise that stresses bone will turn on the remodeling process to increase osteoclast activity simultaneously with increased osteoblastic recruitment.
Additionally there are a huge variety of factors, both intrinsic and extrinsic, that can affect resorption activity. Intrinsic factors are physiologic and pathologic changes that include genetics, peak bone mass accrual in youth, alterations in cellular components, and hormonal, biochemical, and vasculature status. Extrinsic factors are social, behavioral, and pharmacological factors, including nutrition, physical activity, co–morbid medical conditions, and drugs.
How Does Bone Resorption Affect Bone Graft Materials?
As described in this blog, the bone remodeling process maintains homeostasis of our skeletal system and allows the body to access stored minerals like calcium and phosphorus. The remodeling process also plays an important role during bone healing after the implantation of a graft material. In addition to the cellular process described above, the resorption properties of the graft material also play a vital role. During healing, the goal of a bone graft is to provide a scaffold to support new bone formation. Once that function is complete, the graft is no longer needed and is designed to resorb. However, if this happens too quickly, then the graft loses its ability to support new bone formation. Conversely, a bone graft material resorbing too slowly occupies space that could be filled with the patient’s own bone.
Image sources:
- File is licensed under the CC Attribution-Share Alike 4.0 International license. Substantial text alternations, resizing, repositioning, and image replacements were made. Original image available at: https://doi.org/10.3390/cells9092073.
- Tunyogi-Csapo, M. Fibroblast-mediated pathologic bone resorption in ex vivo and in vivo models (2011). Schematic figure is adapted from Clarke B et al. Clin. J. Am. Soc. Nephrol. 2008 Nov 3 Suppl 3: S131-9. Original image available at: https://www.researchgate.net/figure/Multinucleated-osteoclasts-resorb-bone-to-form-resorption-pits-known-as-Howships_fig1_267237031
- Smith T.H., Burger, E.H. and Huyghe, J.M. (2002), A Case for Strain-Induced Fluid Flow as a Regulator of BMU-Coupling and Osteonal Alignment. J Bone Miner Res, 17: 2021-2029. Original image available at: https://doi.org/10.1359/jbmr.2002.17.11.2021
- Chamberlain, A. A preliminary study of microscopic evidence for lactation in cattle. The Zooarchaeology of Fats, Oils, Milk and Dairying (pp.44-49). Repositioning and alternations of color were made. Original image available at: https://www.researchgate.net/figure/Schematic-diagram-of-a-forming-osteon-or-bone-remodelling-unit-Osteoclasts-bone_fig1_275950089
As a recognized leader in advanced bone graft technologies, Biogennix is committed to bringing high-quality educational content to our field. This blog will cover technical topics ranging from basic bone graft science to advanced osteobiologic principles. We’ll also discuss market trends and industry challenges. We thank you for reading and invite you to learn more about us here.